My ankles had disappeared by week 28. I looked down at what used to be my feet and saw swollen, puffy stumps that barely fit into my slip-on shoes. My obstetrician glanced at my legs during a routine checkup and said, “You need compression socks for pregnant women. They’ll help with the swelling and reduce your DVT risk.” I nodded and smiled, but inside I panicked. Aren’t compression socks those tight, constricting things? Is squeezing my already uncomfortable pregnant body really safe? Can pregnant women actually wear compression socks safely?
That concern sent me researching everything about compression socks during pregnancy. I talked to my OB, consulted with a vascular specialist, interviewed dozens of pregnant women who used compression socks, and tested multiple brands throughout my third trimester. What I learned transformed my pregnancy comfort and eliminated the dangerous swelling that had worried my doctor.
Compression socks aren’t just safe during pregnancy; they’re often medically recommended for managing common pregnancy complications. Understanding how to use them correctly ensures you get the benefits without any risks, making the final uncomfortable months of pregnancy significantly more bearable.
The Quick Answer: Are Compression Socks Safe for Pregnant Women?
Yes, compression socks are safe for pregnant women and often medically recommended by obstetricians to reduce leg swelling (edema), prevent varicose veins, reduce DVT (deep vein thrombosis) risk, especially during long flights or bed rest, and improve circulation in the lower extremities during pregnancy. The key is using proper compression levels (15-20 mmHg for general pregnancy use, 20-30 mmHg only with doctor approval), ensuring correct sizing as pregnancy progresses, and avoiding compression that cuts into the belly or restricts blood flow. Most doctors recommend compression socks,s particularly during the second and third trimesters when swelling becomes pronounced, for pregnant women who fly frequently, and for those with jobs requiring prolonged standing or sitting.
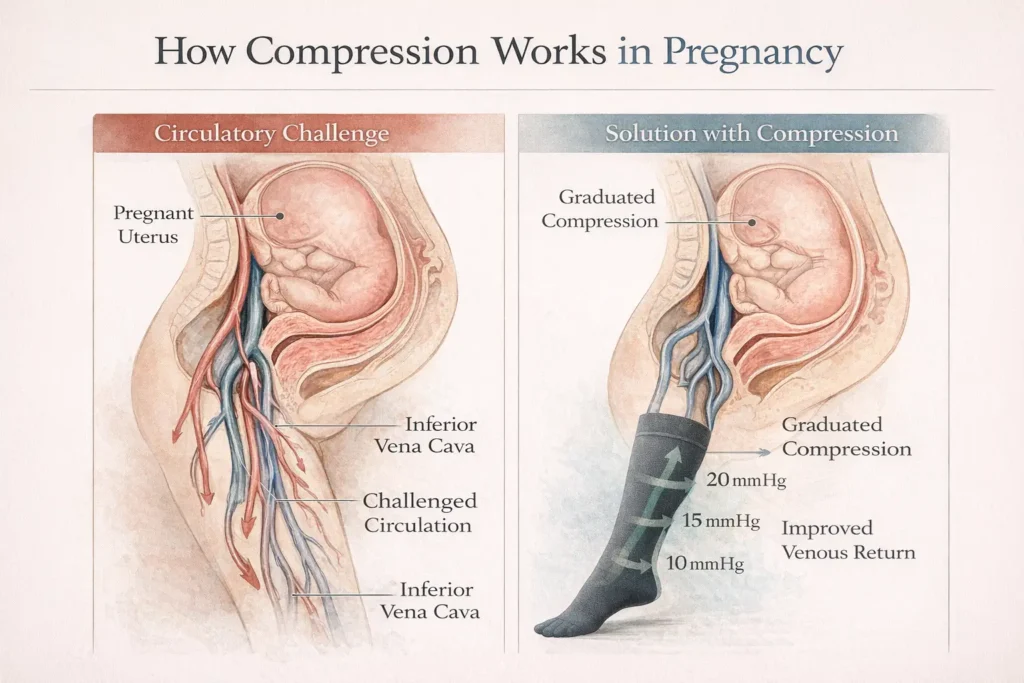
Compression socks work by applying graduated pressure that’s strongest at the ankle and decreases up the leg, helping blood flow back to the heart against gravity. This mechanism is especially beneficial during pregnancy when hormonal changes and increased blood volume make swelling and circulation problems more common.

Understanding Pregnancy Swelling and Circulation Changes
Pregnancy creates dramatic changes in your circulatory system that make swelling and circulation problems extremely common, especially in the later months.
Why Pregnancy Causes Leg Swelling
Your body produces approximately 50% more blood during pregnancy to support your growing baby. This extra blood volume, combined with hormonal changes that relax blood vessel walls, creates perfect conditions for fluid retention and swelling.
Additionally, your growing uterus puts pressure on the large vein (inferior vena cava) that returns blood from your legs to your heart. This pressure slows blood return from the lower extremities, causing blood and fluid to pool in your feet, ankles, and legs.
The hormone relaxin, which loosens ligaments to prepare for childbirth, also affects vein walls. Relaxed vein walls don’t pump blood back to the heart as efficiently, contributing to swelling and increasing varicose vein risk.
When Pregnancy Swelling Becomes Concerning
Some pregnancy swelling is normal. However, certain swelling patterns require medical attention:
Normal swelling: Gradual increase in ankle and foot swelling throughout the day, mild puffiness in hands and face, swelling that improves with rest and elevation, symmetrical swelling in both legs.
Concerning swelling: Sudden, severe swelling in face and hands (possible preeclampsia), swelling in only one leg (possible blood clot), swelling accompanied by severe headaches or vision changes (preeclampsia warning), rapid weight gain from fluid retention (more than 2-4 pounds per week).
If you experience concerning swelling patterns, contact your healthcare provider immediately before trying compression socks or any other treatment.
DVT Risk During Pregnancy
Pregnancy increases your risk of developing dangerous blood clots (deep vein thrombosis or DVT) by 4-5 times compared to non-pregnant women. This increased risk continues through the postpartum period.
DVT risk factors during pregnancy include prolonged bed rest or reduced mobility, long flights or car trips, previous history of blood clots, certain genetic clotting disorders, and obesity or excessive weight gain.
Compression socks help prevent DVT by improving blood flow in leg veins, reducing blood pooling that can lead to clots, and supporting vein walls that pregnancy hormones have relaxed.
For comprehensive information on DVT prevention, see our detailed guide on compression socks for swollen feet.
Are Compression Socks Good for Pregnant Women?
Yes, compression socks provide multiple proven benefits for pregnant women, particularly during the second and third trimesters when circulation challenges become most pronounced.
Reduces Leg and Ankle Swelling
The primary benefit most pregnant women notice is a dramatic reduction in leg and ankle swelling. Compression socks apply graduated pressure that pushes excess fluid out of your leg tissues back into your circulatory system.
Many women report that compression socks allow them to continue wearing regular shoes throughout pregnancy rather than switching to larger sizes to accommodate swollen feet. The swelling reduction also decreases discomfort and heaviness in the legs, which makes walking and standing painful.
Prevents and Manages Varicose Veins
Pregnancy hormones combined with increased blood volume create ideal conditions for varicose veins. These swollen, twisted veins aren’t just cosmetic concerns; they can cause pain, itching, and in severe cases, ulceration.
Compression socks support vein walls and improve blood flow, reducing the pressure that causes veins to swell and become varicose. Women who develop varicose veins during pregnancy often see improvement with consistent compression sock use.
The earlier you start wearing compression socks during pregnancy, the better your chances of preventing varicose veins from developing at all.
Improves Overall Comfort and Mobility
Swollen, heavy legs make simple activities like walking, climbing stairs, or standing to cook dinner exhausting and uncomfortable. Compression socks reduce this heaviness by improving circulation and reducing fluid accumulation.
Many pregnant women report that compression socks make them feel more energetic and able to maintain normal activity levels longer into pregnancy. The improved comfort allows better sleep, more exercise, and generally enhanced quality of life during the challenging final trimester months.
Supports Safe Air Travel During Pregnancy
Flying during pregnancy, especially on long flights, significantly increases DVT risk due to prolonged sitting, cabin pressure changes, and dehydration. Most obstetricians recommend compression socks for pregnant women flying longer than 2-3 hours.
Compression socks counteract the circulation problems that sitting immobile in cramped airplane seats causes. They’re particularly important during the second and third trimesters when DVT risk peaks.
For travel-specific guidance, see our article on compression socks for nurses, which covers similar prolonged standing and circulation challenges.
Are Compression Socks Safe for Pregnant Women?
Compression socks are safe for the vast majority of pregnant women when used correctly. However, understanding proper use and knowing when to consult your doctor ensures you get benefits without any risks.
Medical Consensus on Safety
Major medical organizations, including the American College of Obstetricians and Gynecologists (ACG, support compression sock use during pregnancy for swelling and DVT prevention. Obstetricians routinely recommend compression socks as a first-line, non-pharmaceutical treatment for pregnancy-related leg swelling.
Research shows no evidence that properly fitted compression socks harm pregnant women or developing babies. The gentle, graduated pressure improves maternal circulation without restricting blood flow to the uterus or placenta.
Choosing Safe Compression Levels
Compression socks come in different pressure levels measured in millimeters of mercury (mmHg). Not all compression levels are appropriate for pregnancy:
15-20 mmHg (Mild Compression): Safe for most pregnant women without a doctor’s consultation. Ideal for mild to moderate swelling, preventive use during pregnancy, long flights or car trips, and daily wear for comfort. This is the recommended starting point for pregnancy compression.
20-30 mmHg (Moderate Compression): Requires doctor approval during pregnancy. Used for significant swelling not controlled by 15-20 mmHg, diagnosed varicose veins, and specific medical conditions. Never start this compression level without consulting your obstetrician.
30-40+ mmHg (Firm Compression): Only use with explicit medical prescription. Reserved for serious venous insufficiency or post-surgery recovery. Not typically used during pregnancy except under careful medical supervision.
Most pregnant women get excellent results from 15-20 mmHg compression. Don’t assume more compression is better; higher compression without medical need can actually restrict circulation and cause problems.
Proper Sizing for Pregnancy
Correct sizing is crucial for both safety and effectiveness. Compression socks that are too tight can restrict circulation and cause discomfort. Socks that are too loose provide inadequate compression and slip down.
Pregnancy changes your body rapidly, meaning the size that fits in your second trimester might not work in your third trimester. Measure your ankles and calves every 4-6 weeks to ensure continued proper fit.
Most compression sock brands provide sizing charts based on ankle circumference, calf circumference, and shoe size. Take measurements first thing in the morning, before swelling develops, for the most accurate sizing.
For detailed sizing guidance, see our comprehensive sock sizing guide.
When to Avoid Compression Socks
While safe for most pregnant women, certain conditions require avoiding compression socks or using them only under direct medical supervision:
Peripheral artery disease: Reduced arterial blood flow makes compression dangerous. Your doctor needs to evaluate circulation before approving compression.
Skin infections or open wounds: Compression over infected areas can worsen infections or prevent healing.
Severe peripheral neuropathy: Reduced sensation means you might not notice if compression is too tight or causing problems.
Known allergy to compression sock materials: Some women react to nylon or latex in compression socks. Look for hypoallergenic options.
Certain heart conditions: Uncontrolled congestive heart failure or severe heart disease requires doctor’s evaluation before using compression.
If you have any of these conditions or concerns about whether compression socks are appropriate for your specific pregnancy, consult your obstetrician or a vascular specialist before use.
Do Compression Socks Work for Pregnant Women?
Yes, compression socks demonstrably work for reducing pregnancy-related swelling and circulation problems. The effectiveness comes from their graduated compression design that supports pregnancy-challenged circulatory systems.
How Compression Socks Function During Pregnancy
Compression socks apply pressure that’s strongest at the ankle (typically 15-20 mmHg during pregnancy) and gradually decreases up the leg. This graduated pressure counteracts gravity and helps push blood and fluid from your feet back toward your heart.
During pregnancy, when your growing uterus compresses major blood vessels, and hormones relax the vascular walls, this mechanical assistance becomes particularly valuable. The compression essentially does some of the work your compromised venous system struggles to handle.
Additionally, compression supports weakened vein walls, preventing the ballooning that creates varicose veins. The external pressure helps veins maintain proper shape and function despite pregnancy hormones working against them.
Expected Results and Timeline
Most pregnant women notice swelling reduction within the first week of consistent compression sock use. However, maximum benefits typically take 2-3 weeks of daily wear to become apparent.
What to expect:
- Days 1-3: Initial relief from leg heaviness and discomfort
- Week 1: Noticeable reduction in evening ankle swelling
- Weeks 2-3: Significant improvement in overall leg and foot swelling
- Ongoing: Maintained swelling control and comfort with continued use
The results depend on consistent daily use. Wearing compression socks occasionally provides temporary relief but doesn’t prevent swelling progression like daily use does.
Realistic Limitations
While compression socks work well for pregnancy swelling, they have limitations. They reduce swelling significantly but might not eliminate it, especially during the final weeks of pregnancy. They work best combined with other strategies like leg elevation, reduced sodium intake, adequate hydration, and appropriate rest.
Compression socks prevent and manage mild to moderate varicose veins, but can’t reverse severe varicose veins that existed before pregnancy. They also don’t address the underlying causes of swelling, like preeclampsia, which requires medical treatment beyond compression.
For women with jobs requiring all-day standing, compression socks help but might not completely prevent end-of-day swelling. They reduce it significantly, making discomfort more manageable.
Best Compression Socks for Pregnant Women
Choosing compression socks designed for or appropriate for pregnancy ensures comfort, safety, and effectiveness throughout your changing body.
Key Features for Pregnancy Compression Socks
Adjustable or Expandable Sizing: Look for compression socks that accommodate changing leg sizes throughout pregnancy. Some brands offer maternity-specific lines with extra stretch.
Moisture-Wicking Materials: Pregnancy increases perspiration. Compression socks with moisture-wicking fabrics keep feet comfortable rather than sweaty and clammy.
Seamless or Flat-Seam Construction: Pregnancy makes feet more sensitive. Seamless toes and smooth construction prevent irritation during all-day wear.
Easy to Put On: As pregnancy progresses, bending to put on tight compression socks becomes challenging. Look for socks with features making application easier,r or consider compression sock assist devices.
Non-Binding Tops: The compression sock top should stay up without cutting into your leg or restricting circulation. Wide, soft-top bands work better during pregnancy than narrow elastic bands.
Compression Levels for Different Needs
General Pregnancy Swelling (Most Women):
- 15-20 mmHg knee-high compression socks
- Daily wear from the second trimester through postpartum
- No doctor approval needed for this compression level
Flying During Pregnancy:
- 15-20 mmHg knee-high compression socks
- Wear during flight and for several hours after landing
- Especially important for flights longer than 3 hours
Diagnosed Varicose Veins or Severe Swelling:
- 20-30 mmHg compression (with doctor approval)
- Knee-high or thigh-high, depending on vein location
- Medical-grade compression requiring professional fitting
Preventing Varicose Veins (Family History):
- 15-20 mmHg preventive compression
- Start inthe first trimester before swelling begins
- Continue through pregnancy and the postpartum period
Knee-High vs Thigh-High During Pregnancy
Most pregnant women do well with knee-high compression socks. They’re easier to put on, more comfortable under maternity clothes, and address swelling that primarily affects the lower legs and ankles.
Thigh-high compression might be recommended if you have varicose veins in the thigh area, significant upper leg swelling, or a doctor’s recommendation based on specific conditions. However, thigh-high compression during pregnancy can be uncomfortable as your belly grows, and they’re significantly harder to put on.
Pantyhose-style compression exists for pregnancy, but tends to be uncomfortable around the growing belly. Most women find knee-high socks more practical and comfortable.
For detailed guidance on compression sock types, see our comprehensive article on the best compression socks.
Material Considerations for Pregnancy
Best Materials:
- Moisture-wicking synthetic blends (nylon, polyester, spandex)
- Bamboo blends for softness and natural antimicrobial properties
- Merino wool blends for temperature regulation
Avoid:
- Pure cotton (retains moisture and loses compression when wet)
- Materials you’re allergic to (check labels carefully)
- Very thick materials that make the shoes too tight

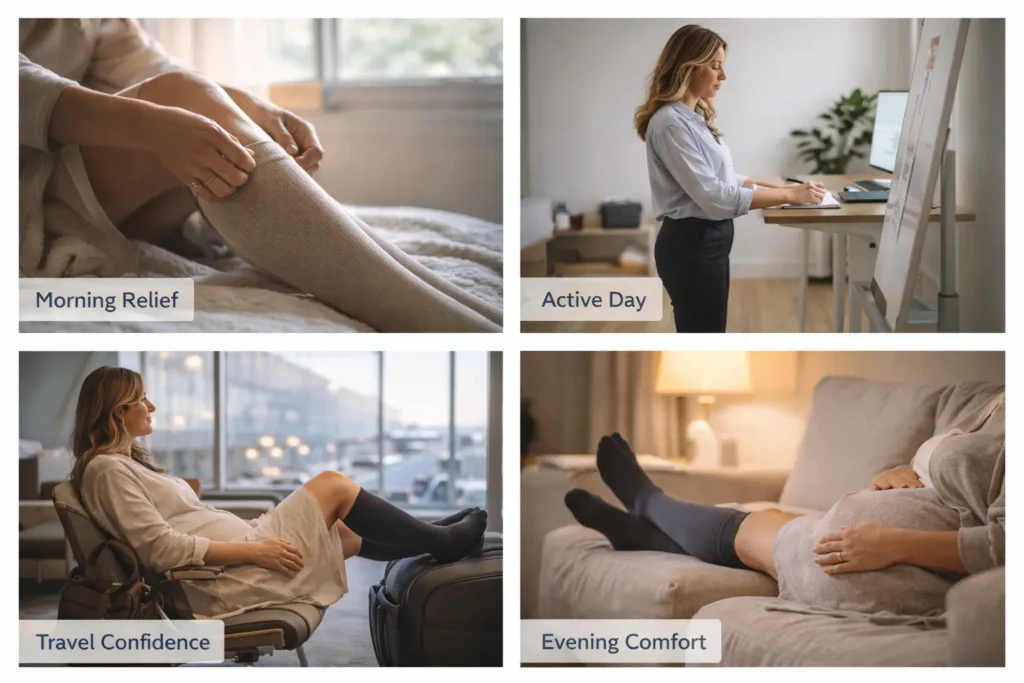
When to Wear Compression Socks During Pregnancy
Timing and consistency of compression sock use affect how well they work and how comfortable they are throughout pregnancy.
Which Trimester to Start
First Trimester: Most women don’t need compression socks yet unless they have risk factors like a history of varicose veins, jobs requiring all-day standing, or previous pregnancies with severe swelling. Starting preventively won’t hurt, butit usually isn’t necessary.
Second Trimester: This is when many women begin noticing leg swelling and should consider starting compression socks. The earlier you address swelling, the better you prevent it from becoming severe.
Third Trimester: Nearly all pregnant women develop some leg swelling by the third trimester. If you haven’t started compression socks yet, beginning now still provides significant benefits for the remaining pregnancy weeks and postpartum recovery.
Daily Wear Schedule
For best results, put compression socks on first thing in the morning before getting out of bed. Swelling is minimal after lying down all night, making this the best time to apply compression and prevent swelling from developing.
Wear compression socks throughout your active day, removing them in the evening when you can elevate your legs and rest. Most women wear them for 8-12 hours daily.
Some women find wearing compression socks during sleep uncomfortable and unnecessary since lying flat naturally improves leg circulation. However, if your doctor specifically recommends overnight compression, follow their guidance.
Special Situations Requiring Compression
Long Flights: Wear compression socks for the entire flight, plus several hours before and after. The cabin pressure changes and immobility significantly increase DVT risk.
Long Car Trips: Similar to flying, extended sitting in cars reduces circulation. Wear compression during the trip and take walking breaks every 1-2 hours.
Work Days: Jobs requiring prolonged standing or sitting benefit from all-day compression sock use. Put them on before work and remove them when you get home.
After Exercise: Some pregnant women find compression socks helpful for recovery after approved pregnancy exercises like walking or prenatal yoga.
Postpartum Use
DVT risk remains elevated for 6-8 weeks postpartum. Many doctors recommend continuing compression sock use during this period, especially if you had significant pregnancy swelling or developed varicose veins.
The postpartum period also involves long periods of sitting while nursing or feeding, making compression socks beneficial for comfort and circulation.
Flying While Pregnant: Compression Sock Importance
Air travel during pregnancy requires special attention to DVT prevention, making compression socks essential rather than optional.
Why Flying Increases Pregnancy DVT Risk
Pregnancy already increases your blood clotting risk. Adding long periods of immobility, cabin pressure changes, and dehydration from dry airplane air creates a dangerous combination.
The American College of Obstetricians and Gynecologists specifically recommends compression stockings for pregnant women on flights longer than 4 hours. Many experts suggest using them on any flight during the second and third trimesters.
Choosing Compression Socks for Flights
For flying, use 15-20 mmHg knee-high compression socks. This provides adequate DVT prevention without being so tight that they become uncomfortable during long flights.
Put compression socks on before leaving for the airport. The journey to the airport, waiting at the gate, and boarding all involve periods of sitting that contribute to DVT risk.
Additional Flight Safety Measures
Compression socks work best combined with other DVT prevention strategies:
- Walk the airplane aisle every 1-2 hours
- Do seated foot and leg exercises
- Stay well hydrated (avoid excessive caffeine)
- Choose aisle seats for easier movement
- Avoid crossing your legs while seated
Common Questions About Pregnancy Compression Socks
Can I wear compression socks to bed while pregnant?
Generally, you don’t need to wear compression socks overnight during pregnancy. Lying flat naturally improves leg circulation. However, if your doctor specifically recommends overnight use, follow their guidance.
How tight should compression socks feel during pregnancy?
Compression socks should feel snug but not painful or restrictive. You should be able to slide a finger under the top band easily. If they leave deep marks, cause pain, or feel numbingly tight, they’re too smal,l or the compression level is too high.
When should I size up my compression socks during pregnancy?
Remeasure your ankles and calves every 4-6 weeks. If measurements increase significantly or your current socks feel too tight, size up. Most women need to size up at least once during pregnancy.
Can compression socks prevent stretch marks on legs?
No, compression socks don’t prevent stretch marks. Stretch marks form in the skin’s deeper layers from rapid stretching, which compression doesn’t address.
Do I need special maternity compression soc, ks or will regular ones work?
Regular compression socks work fine if they fit properly. However, maternity-specific compression socks often feature extra stretch to accommodate changing leg sizes and softer materials for pregnancy-sensitive skin.
Can compression socks harm my baby?
No, properly fitted compression socks don’t harm your developing baby. They improve maternal circulation without restricting blood flow to the uterus or placenta.
Should I wear compression socks on both legs or just the swollen one?
Wear compression on both legs, even if only one is swollen. Pregnancy affects both legs’ circulation, and wearing socks on both maintains balanced circulation.
How do I wash pregnancy compression socks?
Hand wash or machine wash on gentle cycle in cold water. Air dry to preserve compression and elasticity. Never use fabric softener or bleach. For detailed care instructions, see our guide on how to wash grip socks (similar care applies to compression socks).
Can I exercise in compression socks while pregnant?
Yes, compression socks are safe and can be beneficial during approved pregnancy exercises. They improve circulation during activity and may reduce leg fatigue.
What if I can’t bend to put on compression socks?
Use a sock aid device (available at pharmacies) that helps apply compression socks without bending. Or ask your partner to help. Never skip compression socks because application is difficult.
Making the Right Choice for Your Pregnancy
Compression socks provide safe, effective relief for common pregnancy circulation challenges. They reduce dangerous swelling, prevent varicose veins, decrease DVT risk, and improve overall comfort during the physically demanding months of pregnancy.
The key to success is starting early rather than waiting until swelling becomes severe, choosing appropriate compression levels (15-20 mmHg for most pregnant women), ensuring proper sizing that changes as pregnancy progresses, and wearing them consistently throughout active hours.
Always consult your obstetrician before starting compression socks if you have any medical conditions, concerns about their appropriateness, or need help choosing the right compression level. Your doctor can provide personalized guidance based on your specific pregnancy and health situation.
For comprehensive guidance on related compression topics, explore our detailed guides on best compression socks for women, compression socks for swollen feet, and how long you should wear compression socks to understand the complete picture of compression therapy during and after pregnancy.
Questions about using compression socks during your pregnancy? Share your trimester, swelling concerns, and any medical conditions in the comments, and I’ll provide personalized recommendations for safe, effective compression use.